By Tina Teree Baker on Friday, December, 19th, 2014 in Articles. No Comments
Sound knowledge management is an appealing idea. Practically any manager will acknowledge that sound knowledge management is a crucial component for organizational success and will express eagerness at improving knowledge and information flows – at least in principle. However, when the rubber meets the road, many managers are hesitant to accelerate toward solutions that, while appealing in principle, can be complicated to implement. Political, historical, legal, and organizational cultural factors, in addition to practical feasibility, can complicate the integration of sound knowledge management systems into operations that could greatly benefit from them.
The process of building an institutional culture that truly embraces electronic records and knowledge management as a cornerstone of operational workflows can be time-consuming and sometimes challenging. While it is relatively easy to make the case for implementing good knowledge management practices in most organizations (including public health agencies), there are nonetheless a number of significant barriers to implementing such solutions, particularly for public health institutions and other institutions that have a mission to work for the health and well-being of the public.
Where to Start for Sound Knowledge Management
Practical considerations: A sound knowledge management system requires major shifts in time and resources. While an organization benefits from a good knowledge management strategy in the long run, implementing one takes a considerable amount of time – often several years – and investment in expertise. Implementing a new knowledge management program in any institution can be difficult, and even with full implementation, it may take several years to see a noticeable return on the investment. Furthermore, most agencies do not have enough internal expertise in knowledge management for such a comprehensive change, so an outside consultant or significant training for current staff is usually required.
Solution: Get buy-in from managers and top leadership who demonstrate support for employees as they adapt. Cadence’s experience suggests that successful integration of knowledge management into operations moves in a planned, measured and phased approach with active top leadership support. With many public health organizations operating in survival mode, employees need to view embracing knowledge management as a priority and a net gain for themselves and their organization, and vocal support from management goes a long way in fostering this.
Political barriers: Funding of government programs in general, and of public health projects specifically, are highly politicized. One of the primary concerns of public health organizations is budget constraints. Funding situations are rarely stable; budgets are constantly scrutinized for ways to cut costs, be more flexible and operate more efficiently. Agency budgets often shift along with the political landscape, and public health budgets have been targeted in the past as a way to reduce government spending. The current climate of expectations place a premium on a quick and visible return on any financial, time, or political capital investment. They may also be hesitant to acknowledge that their operations “need improvement” by drawing attention to the need for improved knowledge management practices, for fear that this will be misinterpreted as an admission of inefficiency.
Solution: Emphasize to public health leaders that knowledge management is a sound investment. Good knowledge management practices have the potential to help public health organizations fulfill their mandate to save lives and improve health, and they have been demonstrated to save time and resources. A sound knowledge management system does not create more work, but different work – and it improves efficiency and performance in the long term. Knowledge management systems should be promoted as a tool to increase the reach and impact of public health organizations, and to make operations more adaptable to a constantly changing public health landscape.
Historical barriers: Public health programs operate in established “spheres of influence.” Despite years of public health research into why this compartmentalization exists, and efforts to build bridges between established “silos,” many public health organizations have a long history of operating independently in long-established program areas. Rather than encouraging knowledge sharing, they can become “territorial” of what they perceive to be their areas of influence. This leads to duplication of work, as well as wasted funds and efforts.
This is a problem domestically as well as internationally; for example, there are myriad organizations involved in various global health projects, each with its own knowledge management strategies. Organizations with different knowledge management practices may find it challenging to work together to share information. However, the alternative – not having access to critical information – is worse. The following diagram was published in a paper by the Overseas Development Institute that highlights the importance, and the difficulty, of information management and exchange during humanitarian disasters, using the Haiti earthquake as an example.
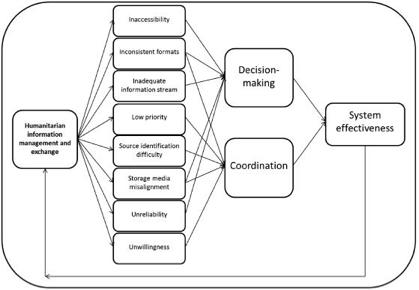
Integrated complexity–information flow impediment framework (Altay and Labonte, 2014).
The above diagram explains that:
a humanitarian agency that finds data inaccessible, inadequate or unreliable will have difficulty in decision-making. On the other hand, for two or more agencies to act together, they need to communicate clearly with each other. If, however, information sharing is accorded a low priority, or if agencies are not willing to share information or they cannot identify the source of the information, then they cannot synchronise their actions. Finally, inconsistent data formats and storage media misalignment would affect both a single agency’s decisions as well as multiple agencies’ coordination, and therefore they are shared impediments between the two factors of system effectiveness.
Solution: Encourage collaboration as a way to administer programs more effectively and increase impact. While the jumping the initial hurdle of synchronizing with other agencies can take time, combining and coordinating the efforts of multiple organizations can accomplish much more in the long term, and it will save time and money by reducing duplicated programs – and allow public health professionals to exchange ideas and expertise. This can, and should, be facilitated by creating a legal climate that encourages such collaboration – for example, clarifying (and, if necessary, relaxing) regulations surrounding authorization for data sharing and information exchange for strictly defined situations, such as emergencies and disaster response. The public health profession could also take steps to standardize the way data is organized and stored – through a set of officially-recognized guidelines, similar to the public health code of ethics initially developed by the Public Health Leadership Society.
Legal barriers: Privacy compliance can be complex and difficult to implement. A significant burden for many public health organizations is compliance with federal, state, and local privacy regulations. These requirements, while necessary to protect patient confidentiality, can be complex and labor-intensive to adhere to. Agency staff may understandably resistant to sanitizing information and implementing a knowledge management system, preferring to maintain limited access and their current practices
Solution: Demonstrate that good knowledge management is universally compatible with privacy regulations. Cadence Group has assisted several government agencies operating in multiple areas with this particular issue. A solid electronic records and knowledge management framework can not only assist with privacy compliance, but can integrate compliance and knowledge capture with regular operations to increase overall efficiency and improve workflows. Furthermore, as mentioned earlier, regulations regarding data privacy and confidentiality can be clarified and modified for certain situations in which greater and more rapid sharing of information is needed.
While many public health institutions and program managers are open to the idea of streamlining sound knowledge management practices into their operations, there are significant barriers to changing the way things are done that would complicate such an undertaking. Simply put, however, the effort to overcome these obstacles is well worth it. The field of public health stands to reap myriad benefits by embracing a culture of effective knowledge and information management. Such a shift would increase the reach and impact of public health programs and allow the public health workforce to grow in skill and confidence. Public health should embrace knowledge management, both for its own sake and for the sake of the populations it serves, in order to work towards better programs and better health.
Written by: Jessica Keralis and Tina Baker
Image by: agsandrew at Depositphotos.com